In a concerning revelation, recent research by Hisham Mehanna, Professor at the Institute of Cancer and Genomic Sciences, University of Birmingham, has identified oral sex as the leading cause of throat cancer in the Western world.
The study highlights a sharp increase in oropharyngeal cancer cases over the past two decades, with many referring to it as an epidemic.
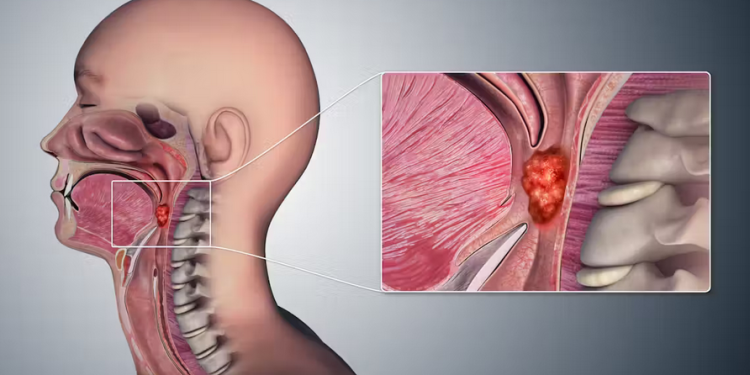
Oropharyngeal cancer, which affects the tonsils and the back of the throat, is primarily caused by the human papillomavirus (HPV).
HPV is also the main cause of cervical cancer, and it has now surpassed cervical cancer in prevalence in both the US and the UK.
Mehanna says the virus is sexually transmitted, and the primary risk factor for developing oropharyngeal cancer is the number of lifetime sexual partners, particularly those involving oral sex. Individuals with six or more lifetime oral sex partners are 8.5 times more likely to develop oropharyngeal cancer compared to those who have not practised oral sex.
Mehanna notes that behavioural studies indicate that oral sex is widely practised, with 80% of adults in the UK reporting having engaged in it at some point in their lives. Despite this high prevalence, only a small number of these individuals develop oropharyngeal cancer.
The prevailing theory suggests that while most people can clear HPV infections naturally, a small number cannot, possibly due to a defect in their immune system, allowing the virus to replicate continuously and potentially cause cancer.
To combat this growing health issue, Mehanna says many countries have implemented HPV vaccination programmes for young girls to prevent cervical cancer. Increasing evidence suggests that these vaccines may also be effective in preventing HPV infections in the mouth, thus reducing the risk of oropharyngeal cancer.
Additionally, boys are benefiting from herd immunity in regions with high vaccine coverage among girls. Countries such as the UK, Australia, and the US have now extended their HPV vaccination recommendations to include young boys, adopting a gender-neutral vaccination policy.
However, Mehanna indicates that universal vaccination policies do not guarantee full coverage. Vaccine hesitancy and opposition due to safety concerns or fears of promoting promiscuity remain significant barriers. The COVID-19 pandemic has further complicated efforts to reach young people and has contributed to a rise in anti-vaccine attitudes.
Professor Mehanna’s findings underscore the urgent need for increased awareness and vaccination coverage to address this growing health threat. Public health officials and policymakers

Comments are closed.